An estimated 1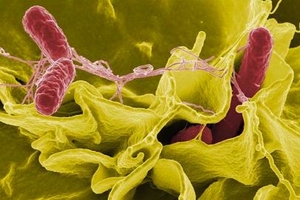 .2 million Salmonella-related illnesses occur each year in the United States. Approximately 400 people die.
.2 million Salmonella-related illnesses occur each year in the United States. Approximately 400 people die.
While Salmonella is most often associated with poultry products, outbreaks are linked to a wide variety of sources, including contaminated ground beef, fruits and vegetables, dog food, turtles and hedgehogs.
Scientists first identified Salmonella as a human pathogen in the late 19th Century. While monitoring and tracking methods have improved, the bacteria continue to cause significant issues and foodborne disease outbreaks.
There are more than 2,000 strains of Salmonella. The different strains of Salmonella are categorized based on the specific antigen set of each. Antigens are substances that stimulate the body to fight pathogens. These antigen-based subsets are called serotypes.
Here is a list of the five most common serotypes in order of prevalence in relation to foodborne illnesses.
Salmonella Enteritidis
Enteritidis is the most common strain of Salmonella in our food supply. The increased prevalence in poultry products made Salmonella Enteritidis a food-safety issue in the 1970s. It is the serotype most often associated with poultry.
Prior to that, Salmonella Pullorum and Salmonella Gallinarum were endemic in poultry flocks, according to research by Steven Ricke at the University of Arkansas. However, these strains were minimized through aggressive eradication programs.
Salmonella Enteritidis infects the gastrointestinal tract of poultry. Salmonella is passed from bird to bird in several ways, most commonly through fecal matter. Poultry have a tendency to scratch through dirt and manure, and hen they do this, they can become infected if the manure has live Salmonella bacteria in it.
When poultry are slaughtered, Salmonella is spread from the intestinal tract onto the meat. Salmonella is also found in the ovaries of laying hens and thus passed on through shell eggs.
There are several testing programs in place to detect and reduce the threat of this strain in the poultry meat and shell egg supply.
Based on U.S. Centers for Disease Control and Prevention data, Enteritidis outbreaks since 2010 were linked to shell eggs, alfalfa sprouts, pine nuts and ground beef.
Salmonella Typhimurium
Typhimurium is the second most common serotype associated with foodborne illness and the third most frequently identified with chicken.
This serotype is also linked to ground beef, pork and other poultry products. Beef researchers say that Salmonella Typhimurium in ground beef could be the biggest food safety issue facing the beef industry today.
Typhimurium has proven to be antibiotic-resistant, which makes eliminating the pathogen from food products very challenging.
Beef researchers are looking into pre-harvest interventions such as vaccinations and probiotics to reduce Typhimurium in cattle.
Unlike other serotypes that populated the intestinal tract of animals, Typhimurium might be in the lymph system of cattle. Research is ongoing.
The CDC list of outbreaks associated with Typhimurium since 2006 show the following as sources: Ground beef, hedge hogs, cantaloupes, peanut butter, tomatoes and African dwarf and water frogs.
Salmonella Newport
Newport is currently the third most common Salmonella serotype associated with foodborne illness.
This strain is most often associated with turkey products. Like Typhimurium, it has been determined to be antibiotic-resistant.
In the fall of 2012, Salmonella Newport and Typhimurium were found in cantaloupe. The outbreak led to three deaths and more than 250 illnesses in 24 states.
In addition to cantaloupe, live poultry and alfalfa sprouts have been linked to Newport outbreaks since 2010.
Salmonella Javiana
Javiana is the fourth most common serotype associated with foodborne illness. A report on Salmonella serotypes from the Food Safety and Inspection Service (FSIS), the food safety arm of the U.S. Department of Agriculture, indicated this strain is not often associated with products regulated by the agency.
This serotype is associated with exposure to amphibians in the Southeast U.S. It has also been linked to contaminated mozzarella cheese, watermelon, bass, poultry, lettuce and tomatoes.
CDC has not reported a multistate outbreak associated with Javiana since 2006. However, in January 2011 there was a death at a retirement home in Maine attributed to Javiana in a food product.
Salmonella Heidelberg
Heidelberg is the fifth most common Salmonella serotype associated with foodborne illness and the second most frequently associated with human health issues and poultry, according to a recent report from FSIS.
Salmonella Heidelberg has caused recent poultry recalls and foodborne illness outbreaks. In March of this year, 128 illnesses in 13 states were linked to Heidelberg in chicken meat. It is also found in shell eggs.
However, current FDA guidelines are designed to limited Salmonella Enteritidis and do not specifically address Heidelberg.
“Heidelberg [in eggs] is a new threat for the CDC and FDA to deal with,” said Paul Patterson, professor of poultry science at Pennsylvania State University. “Testing isn’t specifically designed for this strain, but if a farm is testing and has knowledge it is present, they are obligated to act.”
John Sheehan, director of FDA’s Division of Plant and Dairy Food Safety, said that Heidelberg is not a new issue for the agency. He noted it was mentioned in 2004 as a major challenge.
While the new egg safety rule that went into effect in 2010 primarily addresses Enteritidis issues, he said inspectors are trained to look for Heidelberg as well.
“The egg safety rule is all about Salmonella Enteritidis, and our goal is to eliminate Salmonella Enteritidis as a source of foodborne illness,” Sheehan said. “But if we learn that Heidelberg is present, we cannot ignore it. There is transference potential, and it can’t be ignored in an egg-production environment.”
Sheehan noted that FDA sent a warning letter to an egg producer whose facilities tested positive for Heidelberg in the fall of 2012.
The letter went to Centrum Valley Farms in Iowa. Centrum just happens to be the new owner of Wright Country Egg and Hillandale Farms, the sources of more than 500 million Enteritidis-contaminated eggs involved in the largest egg recall in U.S. history.
FDA officials noted that two of Centrum Valley’s hen houses tested positive for Heidelberg during an inspection. Eggs were tested and came back negative for Heidelberg. No eggs were distributed until the negative results were received and the farm received the go-ahead from FDA.
 .2 million Salmonella-related illnesses occur each year in the United States. Approximately 400 people die.
.2 million Salmonella-related illnesses occur each year in the United States. Approximately 400 people die.While Salmonella is most often associated with poultry products, outbreaks are linked to a wide variety of sources, including contaminated ground beef, fruits and vegetables, dog food, turtles and hedgehogs.
Scientists first identified Salmonella as a human pathogen in the late 19th Century. While monitoring and tracking methods have improved, the bacteria continue to cause significant issues and foodborne disease outbreaks.
There are more than 2,000 strains of Salmonella. The different strains of Salmonella are categorized based on the specific antigen set of each. Antigens are substances that stimulate the body to fight pathogens. These antigen-based subsets are called serotypes.
Here is a list of the five most common serotypes in order of prevalence in relation to foodborne illnesses.
Salmonella Enteritidis
Enteritidis is the most common strain of Salmonella in our food supply. The increased prevalence in poultry products made Salmonella Enteritidis a food-safety issue in the 1970s. It is the serotype most often associated with poultry.
Prior to that, Salmonella Pullorum and Salmonella Gallinarum were endemic in poultry flocks, according to research by Steven Ricke at the University of Arkansas. However, these strains were minimized through aggressive eradication programs.
Salmonella Enteritidis infects the gastrointestinal tract of poultry. Salmonella is passed from bird to bird in several ways, most commonly through fecal matter. Poultry have a tendency to scratch through dirt and manure, and hen they do this, they can become infected if the manure has live Salmonella bacteria in it.
When poultry are slaughtered, Salmonella is spread from the intestinal tract onto the meat. Salmonella is also found in the ovaries of laying hens and thus passed on through shell eggs.
There are several testing programs in place to detect and reduce the threat of this strain in the poultry meat and shell egg supply.
Based on U.S. Centers for Disease Control and Prevention data, Enteritidis outbreaks since 2010 were linked to shell eggs, alfalfa sprouts, pine nuts and ground beef.
Salmonella Typhimurium
Typhimurium is the second most common serotype associated with foodborne illness and the third most frequently identified with chicken.
This serotype is also linked to ground beef, pork and other poultry products. Beef researchers say that Salmonella Typhimurium in ground beef could be the biggest food safety issue facing the beef industry today.
Typhimurium has proven to be antibiotic-resistant, which makes eliminating the pathogen from food products very challenging.
Beef researchers are looking into pre-harvest interventions such as vaccinations and probiotics to reduce Typhimurium in cattle.
Unlike other serotypes that populated the intestinal tract of animals, Typhimurium might be in the lymph system of cattle. Research is ongoing.
The CDC list of outbreaks associated with Typhimurium since 2006 show the following as sources: Ground beef, hedge hogs, cantaloupes, peanut butter, tomatoes and African dwarf and water frogs.
Salmonella Newport
Newport is currently the third most common Salmonella serotype associated with foodborne illness.
This strain is most often associated with turkey products. Like Typhimurium, it has been determined to be antibiotic-resistant.
In the fall of 2012, Salmonella Newport and Typhimurium were found in cantaloupe. The outbreak led to three deaths and more than 250 illnesses in 24 states.
In addition to cantaloupe, live poultry and alfalfa sprouts have been linked to Newport outbreaks since 2010.
Salmonella Javiana
Javiana is the fourth most common serotype associated with foodborne illness. A report on Salmonella serotypes from the Food Safety and Inspection Service (FSIS), the food safety arm of the U.S. Department of Agriculture, indicated this strain is not often associated with products regulated by the agency.
This serotype is associated with exposure to amphibians in the Southeast U.S. It has also been linked to contaminated mozzarella cheese, watermelon, bass, poultry, lettuce and tomatoes.
CDC has not reported a multistate outbreak associated with Javiana since 2006. However, in January 2011 there was a death at a retirement home in Maine attributed to Javiana in a food product.
Salmonella Heidelberg
Heidelberg is the fifth most common Salmonella serotype associated with foodborne illness and the second most frequently associated with human health issues and poultry, according to a recent report from FSIS.
Salmonella Heidelberg has caused recent poultry recalls and foodborne illness outbreaks. In March of this year, 128 illnesses in 13 states were linked to Heidelberg in chicken meat. It is also found in shell eggs.
However, current FDA guidelines are designed to limited Salmonella Enteritidis and do not specifically address Heidelberg.
“Heidelberg [in eggs] is a new threat for the CDC and FDA to deal with,” said Paul Patterson, professor of poultry science at Pennsylvania State University. “Testing isn’t specifically designed for this strain, but if a farm is testing and has knowledge it is present, they are obligated to act.”
John Sheehan, director of FDA’s Division of Plant and Dairy Food Safety, said that Heidelberg is not a new issue for the agency. He noted it was mentioned in 2004 as a major challenge.
While the new egg safety rule that went into effect in 2010 primarily addresses Enteritidis issues, he said inspectors are trained to look for Heidelberg as well.
“The egg safety rule is all about Salmonella Enteritidis, and our goal is to eliminate Salmonella Enteritidis as a source of foodborne illness,” Sheehan said. “But if we learn that Heidelberg is present, we cannot ignore it. There is transference potential, and it can’t be ignored in an egg-production environment.”
Sheehan noted that FDA sent a warning letter to an egg producer whose facilities tested positive for Heidelberg in the fall of 2012.
The letter went to Centrum Valley Farms in Iowa. Centrum just happens to be the new owner of Wright Country Egg and Hillandale Farms, the sources of more than 500 million Enteritidis-contaminated eggs involved in the largest egg recall in U.S. history.
FDA officials noted that two of Centrum Valley’s hen houses tested positive for Heidelberg during an inspection. Eggs were tested and came back negative for Heidelberg. No eggs were distributed until the negative results were received and the farm received the go-ahead from FDA.





